Metastatic liver cancer occurs when tumors spread to the liver from other parts of the body. The cancers most often come from colorectal, lung or breast primary cancers.
Doctors can treat liver metastases to relieve symptoms and extend life expectancy. Treatment options include alcohol injection, using heat to destroy the cancer cells (radiofrequency ablation or microwave ablation), radiation therapy and chemotherapy.
Symptoms
Cancer cells can spread (metastasize) to other parts of the body through the bloodstream or lymph vessels. When they reach a new area, the cancer cells may grow and form a new tumor, or metastasis. When cancer spreads to the liver, it is called metastatic liver disease.
The symptoms of metastatic liver cancer depend on the location of the spread and the type of cancer that originated in another part of the body. Some people with cancer that has spread to the liver have no symptoms at all. The most common symptom of metastatic liver cancer is fatigue. Cancer treatments can also cause loss of appetite and other side effects that can affect how much energy a person has.
Liver metastases are most often caused by cancers that started in the colon or breast. But they can also start in the esophagus, pancreas, gallbladder, skin, kidney and lung. Because the liver receives both the hepatic artery and the portal vein, it is a common site for metastases from a variety of abdominal cancers.
If cancer has spread to the lungs, the symptoms can include a cough, breathing difficulty and fluid buildup in the lungs (pleural effusion). In addition, some people with lung metastases develop a tumor on the outside of the chest wall called a pulmonary nodule.
Symptoms of liver metastases can be very vague and difficult to recognize, especially in early stages. Because these symptoms resemble other medical conditions or problems, it’s important to talk with your doctor about any unusual changes you experience.
At Memorial Sloan Kettering, we have a team of specialists that are experienced in diagnosing and treating liver metastatic cancer. We take a multidisciplinary approach with medical oncologists, radiation oncologists and interventional radiologists as well as surgical oncologists.
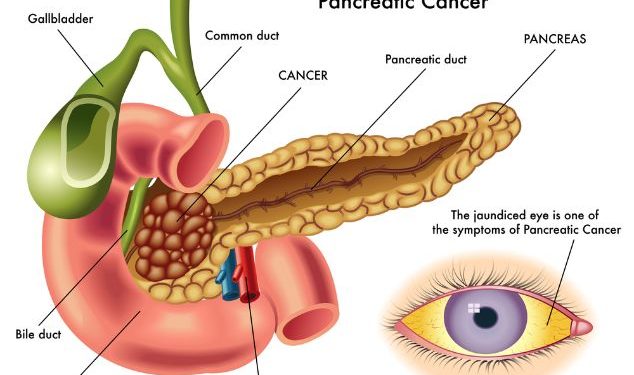
Symptoms of liver metastases can vary, but they typically include fatigue and weight loss. Other possible symptoms include pain in the abdomen, nausea and vomiting, abdominal fluid (ascites) and jaundice (yellowing of the skin and whites of the eyes). If a patient has these symptoms, their healthcare provider will do tests to find out where the cancer started.
Diagnosis
It can be difficult to tell when cancer has spread to the liver. It is important to let a doctor know if you have any new symptoms, including fatigue, so that they can help you find out what is happening. Memorial Sloan Kettering doctors who specialize in metastatic liver cancer are experts at recognizing these symptoms and getting them diagnosed quickly.
Liver metastases occur when a cancer that starts in another part of the body spreads to the liver through the blood or lymphatic system. Cancer that begins in the liver and is not metastatic is called primary liver cancer or hepatocellular carcinoma.
The diagnosis of liver metastases usually is made based on the results of imaging tests and a biopsy. If the tumors are small, they may not show up on these tests. A biopsy involves inserting a needle into the liver to remove tissue for examination under a microscope. Doctors also may use a thin tube with a camera attached (laparoscope) to look at the liver through an incision in the belly.
If the cancer has already spread beyond the liver to other parts of the body, a diagnosis is usually made from the symptoms and the results of blood and urine tests. The type of treatment used for a person with metastatic liver cancer depends on where the cancer started and whether it is curable.
The outlook for a person with metastatic liver cancer is poor. The cancer is not always cured, but treatments can help reduce symptoms and slow the growth of the tumors.
Metastatic liver cancer often develops from cancers that start in the lungs, breasts, large intestine, pancreas, or stomach. It can also spread from leukemia (cancer of white blood cells) and lymphoma, especially Hodgkin lymphoma.
If a person has only one area of liver metastasis, surgery might be possible. The surgery, called liver resection, removes the part of the liver with the tumor. Chemotherapy drugs might be used before or after surgery to destroy any remaining cancer cells. Doctors may also give a treatment called chemoembolization. This procedure involves inserting a tube into an artery in the groin and sending cancer-killing medicine through it to the liver. This blocks blood flow to the part of the liver with the tumor, which “starves” the tumor of oxygen and kills it.
Treatment
Metastatic liver cancer can be more difficult to cure than primary tumors that start in the liver. But we have many treatment options to control the growth of your tumors, relieve symptoms, and improve your quality of life. Treatment depends on the type of cancer that spread to your liver, where it started, and how much of your liver is affected.
The most common treatment for metastatic cancer in the liver is chemotherapy. Chemotherapy uses drugs that circulate through your bloodstream to destroy cancer cells throughout the body. It may be given intravenously (through a needle in a vein) or by mouth. The type and combination of chemotherapy drugs you receive will depend on where your cancer started and how much of your liver is affected.
In some cases, we use ablation therapy to kill tumors that are not responding to chemotherapy or when a patient cannot have surgery or radiation. Ablation therapies include radiofrequency ablation and microwave ablation, which use special needles inserted into the tumor or through an incision in the skin to heat the tissue and kill cancer cells. We also use percutaneous ethanol injection, in which a small needle is used to inject ethanol directly into the tumor to kill cancer cells.
Surgical removal of the liver tumor is possible, but the extent of the surgery will be limited by how large the tumors are and by how healthy your liver is. If the cancer has spread widely, we may recommend a partial hepatectomy in which a wedge or entire lobe of the liver is removed and some healthy liver tissue takes over its functions. We may also offer a liver transplant if the tumor is causing hepatobiliary complications like jaundice.
Another option is transarterial chemoembolization, in which we use a catheter (tube) to deliver chemotherapy and a substance that blocks the supply of blood to a liver tumor (an embolic agent). This prevents the cancer from getting the oxygen and nutrients it needs to grow.
We also offer supportive care services for people who are dealing with the emotional, social, and practical challenges of living with liver cancer. These can include support groups, in-person and online, for patients and their families, and a variety of counseling and educational programs.
Prevention
There is no known way to prevent liver cancer that has already spread from another place in the body. But you can take steps to lower your risk of developing primary liver cancer.
The most common type of primary liver cancer, hepatocellular carcinoma, starts in the cells that line the bile ducts, tubes that carry bile from the liver to the intestines. It’s most commonly found in people with cirrhosis, which is caused by long-term damage to the liver due to alcohol use or other conditions, like nonalcoholic steatohepatitis (NASH).
People with chronic infections with hepatitis C virus (HCV) or hepatitis B virus (HBV) have an increased risk of developing liver cancer. Both HCV and HBV can cause liver inflammation, which can lead to scarring that can become cancerous. Routine hepatitis C treatment in adults with a sustained virologic response (SVR) reduces cirrhosis, a major risk factor for hepatocellular carcinoma and other types of liver cancer.
In addition to avoiding alcohol, you should get regular screening for hepatitis A and B. You can find out if you have these infections through blood tests at your doctor’s office.
You should also get a healthy diet. Eat plenty of fruits and vegetables, lean proteins and whole grains. Try to avoid high-fat foods and processed meats. Exercise regularly. This can help you maintain a healthy weight and reduce your risk for obesity, which is linked to an increased risk of liver cancer.
If you do have a health condition that increases your risk for liver cancer, see a specialist. NYU Langone doctors can identify conditions that may increase your risk and recommend lifestyle changes to decrease your chances of getting cancer.
Talk to your family and friends about the importance of good health habits. They can be a great source of support and offer practical help, such as watching your children if you have to go to the hospital. Also, keeping your close relationships strong can be helpful when dealing with a serious illness. And they can provide emotional support when you need it. This support can be especially important if you’re diagnosed with a cancer that is difficult to treat, such as metastatic liver cancer.